Great power of coagulation which drastically reduces blood loss.
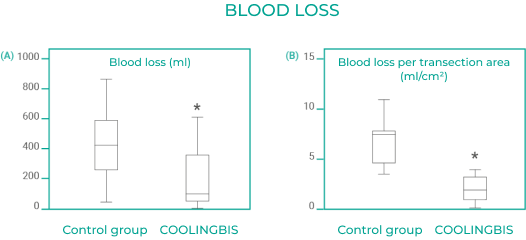
Results of the randomised clinical trial to evaluate the impact of COOLINGBIS® on intraoperative blood loss during liver resection (AGEMED 312/08 EC)4.
The box diagram shows blood loss during transection (A) and blood loss per transection area (B) in the control group, in which haemostasis is obtained using conventional techniques, and in the MRFC (monopolar radiofrequency coagulation) group, in which haemostasis is obtained using COOLINGBIS®. The box represents the interquartile range containing 50% of the values. The whiskers are lines that extend from the box to the larger and smaller values. The line in the box indicates the median. Both results are statistically significant (*p<.05).
On the basis of the argument that remaining malignant cells in the hepatic remnant are responsible for tumour relapse, M. Villamonte, F. Burdío, E. Pueyo et. al. aimed to demonstrate that additional coagulation of the hepatic surface with an efficient RF-based device (COOLINGBIS®) not only successfully achieved hemostasis but also had a favorable effect on local recurrence5.

Figure shows the Kaplan-Meier curve of local hepatic recurrence-free survival in patients with liver tumors with distance from the tumour to resection margin <10 mm (Log-rank test p=0.049).
The estimated 1-, 3-, and 5-year local recurrence free survival of the control and COOLINGBIS group patients were 93.5%, 86.0%, 81.0% and 98.8%, 97.2%, 91.9% respectively (p=0.049).
The COOLINGBIS® Group was significantly associated with reduced local recurrence5.
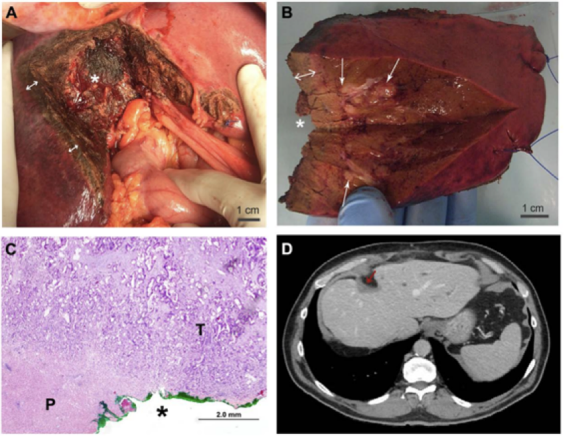
(A) The liver after removal of the sample; the coagulated tissue (double arrow) and the resection margin (*) can be seen.
(B) The liver sample from the same patient; the resection margin and the thickness of the coagulated tissue (double arrow) which is in contact with the metastasis (arrow), can be seen. The * shows the correct position of the sample.
(C) Histological section of the resection margins of the sample (use the asterisk for the correct position). The resection margin is marked with green ink. You can see the tumour ( T ) and the coagulated parenchyma ( P ) in contact with the margin. The coagulated tumour did not prevent the correct evaluation of the invasion of the margins.
(D) CT scan of the same patient 56 months after liver resection, no signs of liver local recurrence are observed. The remaining ablated tissue at the margin can be noted (red arrow)4.
Significant reduction of postoperative stay (days).

Results of consecutive patients in the COOLINGBIS® series in reference study 312/08/EC1. Patient nº3, after liver transection and in the same surgical act, underwent anterior resection of the rectum with hysterectomy and partial cystectomy due to invasive colon neoplasia of these organs.
The patient was operated 11 days later as a result of a leakage of colorectal anastomosis from which he evolved favourably.
Coagulative necrosis plane just after resection:

Transection plane 3 months after resection:

1. Burdío, F. et al. A new single-instrument technique for parenchyma division and hemostasis in liver resection: A clinical feasibility study. Am. J. Surg. 200, e75–e80 (2010).
2. Stavrou, G. A., Donati, M., Fruehauf, N. R., Flemming, P. & Oldhafer, K. J. Liver resection using heat coagulative necrosis: Indications and limits of a new me- thod. ANZ J. Surg. 79, 624–628 (2009).
3. Weber, J. C. et al. New technique for liver resection using heat coagulative necrosis. Ann. Surg. 236, 560– 563 (2002).
4. Quesada, R. et al. Impact of monopolar radiofrequency coagulation on intraoperative blood loss during liver resection: a prospective randomised controlled trial. Int. J. Hyperth. 33, 135–141 (2017).
5. Villamonte, M. et al. The impact of additional margin coagulation with radiofrequency in liver resections with subcentimetric margin: can we improve the oncological results? A propensity score matching study. Eur. J. Surg. Oncol. 25–29 (2021) doi:10.1016/j.ejso.2021.06.008.
6. Quesada, R. et al. The impact of radiofrequency-assisted transection on local hepatic recurrence after resection of colorectal liver metastases. Surg. Oncol. 26, 229–235 (2017).
COOLINGBIS is a monopolar electrosurgical sealing dissector for soft tissues, intended for haemostatic sealing, coagulation and cut (models with blade).
> COOLINGBIS complies with European standards for the sale of medical devices
> CE European Directive 93/42/CEE (ON 1984)
> UNE-EN ISO 13485:2018
Vecmedical Spain S.L.
Pol. Ind. Can Milans, nave 9
Montcada i Reixac, Barcelona, 08110
Tel. +34 935725015
E-mail: vecmedical@vecmedical.com
Copyright Vecmedical / Legal Advice / Cookies / Privacy Policy